- Home
- Women's Infections
- Recurring Yeast Infection
Recurring Yeast Infection and How to Get Rid of It For Good
Updated 11/02/2021
Medically reviewed by Dr. Atmika Paudel, PhD - Written by Dan Jackowiak Nc, HHP and Dr. Shalaka Samant, PhD
Dr. Atmika Paudel, PhD says... The information presented in this article about recurring yeast infections, their causes and potential remedies is medically correct.
If you get a recurring yeast infection at certain times of the month you are not alone. Many women get them right at the start of ovulation and they last until menstruation, and then go away only to return again at ovulation the next month. Other women get them at other times of their cycle but this is not as common.
Getting rid of them can be a very frustrating experience. Usually over-the-counter creams are used and initially they seem to work. So you stop and then next month the yeast is back with a vengeance.
At this point, most women will make a trip to the doctor for a
prescription of Diflucan which also seems to work. A month goes by and
here it is again with the itching, burning and cottage cheesy discharge.
In these causes, you have to fix the underlying causes or you will never have any relief.
Dr. Shalaka Samant, PhD says...
Vaginal infections caused by Candida are extremely common. At least 75% of women suffer once in their lifetime from one episode of a Candida infection (1).
1. Fungal vulvovaginitis. Current Opinion in Obstetrics and Gynecology. 3(6):849–852, DECEMBER 1991. PMID: 1818723
What Causes Recurring Yeast Infections?
There are a few primary causes of these vaginal yeast infections.
1. You have an over growth in your intestine and are simply re-infecting yourself month after month.
Studies have shown that if yeast is detectable in your vagina, it will usually be found in your stool. The close proximity of the anus and vagina allows yeast to transfer from the colon and give you a vaginal yeast infection.
Anal itching is a good indicator that this is what is happening although anal itching can also be pinworms or other parasites.
2. You have a hormone imbalance, mostly too much estrogen.
Yeast becomes dependent on estrogen in the vagina because estrogen controls vaginal glycogen levels. If there is an excess, you will have an excess of sugar as well and this sugar feeds yeast. Excess estrogen also has an effect on your immune system reducing its function.
3. You are being infected by your sexual partner.
About 30% of people have candida yeast in their mouths and it is possible to acquire an infection during oral sex if your partner is one of those people. Also, about 15% of men will have yeast growing on their penis and present in the seminal fluid.
It is not a bad idea to treat your partner while treating yourself to rule out this possibility.
Dr. Shalaka Samant, PhD says...
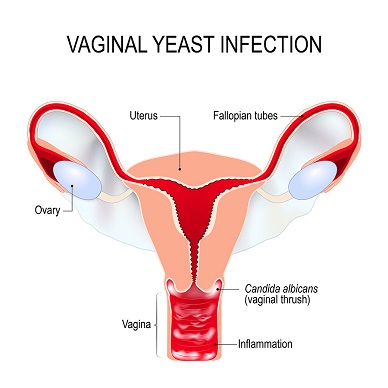
Some illnesses increase the risk of recurring vaginal yeast infections. These include diabetes and other diseases that weaken the immune system (2). Various medications can increase the risk too, such as antibiotics, steroids, hormone therapy, radiotherapy and chemotherapy. Other factors that increase the risk of vaginal yeast infections include stress, washing your genitals with soap, wearing synthetic and tight clothes, sweating and using “non-breathable” panty liners or sanitary pads. These things allow the yeast to thrive, leading to an inflammation.
2. Vaginal yeast infection (thrush): Overview. InformedHealth.org. Created: June 19, 2019
How to Determine if You Have Intestinal Yeast?
The only way to find out if it is in your intestine is to be stool tested and on the Candida Tests page I have listed the best tests to use.
If you do not do the stool test but do occasionally have anal itching, you can get a pretty good idea if it is intestinal by taking the Yeast Infection Questionnaire. If you score high on that test then it would be safe to assume it is intestinal as well.
You can also check the symptoms page here. If you find that many of those symptoms are a problem for you, especially:
A poor appetite
Chronic fatigue
Constipation
Frequent intestinal gas
Chronic hives
Bloating and indigestion
Acne and other skin rashes
Have an excessive craving for sugars
Then you probably could assume you have too much yeast in your intestine, especially if you scored high on the questionnaire.
Dr. Shalaka Samant, PhD says...
Symptoms include pruritis, burning, irritation, soreness, and a change in discharge. A large majority of these infections are uncomplicated and respond well to anti-fungal therapy. However, about 5-10% of the patients, suffer from at least four episodes of Candida infection a year (3). They are diagnosed as having a recurrent infection.
Candida albicans is the most common cause of recurring yeast infections; although non-albicans species (4), which are generally less susceptible to antifungals commonly used to treat yeast infections, can also be found as the causative agent.
3.
Facts and myths on recurrent vulvovaginal candidosis—a review on
epidemiology, clinical manifestations, diagnosis, pathogenesis and
therapy. International Journal of STD and Aids. First Published August
1, 2002
4. Epidemiology
of recurrent vulvovaginal candidiasis: identification and strain
differentiation of Candida albicans. J Infect Dis. 1986 Aug;154(2):358-63.
What to do About Intestinal Yeast
If you have intestinal yeast over growth and vaginal infections, it is considered a systemic yeast infection. Systemic yeast is simply having an active infection in two or more places at the same time.
Make sure you follow the candida yeast diet. There is no point in feeding your recurring yeast infection if it came from the intestine originally, through the anus, and infected your vagina.
As far as taking yeast killing supplements, the best thing to do is to follow the 3-Step Plan here or the Systemic System I have laid out here.
Dr. Shalaka Samant, PhD says...
Extragenital reservoirs for Candida such as the intestine and mouth have often been implicated in recurring yeast infections (5). C. albicans lives in harmony with the rest of the host’s fecal flora and minor perturbations such as pregnancy or broad-spectrum antibiotic usage might alter the delicate balance and cause the Candida to become pathogenic. Frequent antibiotic use decreases protective vaginal flora and allows colonization by Candida species. This is where probiotic supplements or foods like yogurt with active cultures may help.
5. Recurrent vaginal candidiasis. Importance of an intestinal reservoir. JAMA. 1977 Oct 24;238(17):1836-7.
What if You Don't Have Intestinal Yeast
If you don't have intestinal yeast, then while you are correcting the hormone problems, I would take one of the enzyme formulas I talk about here.
These enzyme formulas are designed to eat the cell wall of candida
yeast effectively killing it with very little if any die-off reactions. Biofase
is the best because it also contains enzymes that eat through the
biofilm yeast builds around itself as a means of protection. Sometimes
results
are felt the very first day.The recommended dose is three capsules one
hour before breakfast and at bedtime.
You should also take Profase
because most of the bacteria in this probiotic are found in the vagina
and all are found in the human body. These bacteria have multiple
studies proving they are more effective against yeast than your typical
probiotic strains. More potent than Lactobacillus acidophilus, L. rhamnosus, L reuteri, Lactobacillus salivarius, Bifidobacteriam infantis, etc. Go check the studies yourself, I have them posted. Take two capsules of Profase with Biofase twice a day.
I also suggest that Floraphage be taken with Profase or any other probiotic you decide to try. Floraphage has been proven to increase bacteria levels 24x above control, so one capsule of Profase can turn into 720 billion. It will also help your good bacteria to come back so you can prevent these infections in the future.
How to Find Out if Estrogen is Causing Your Infection
The best thing for you to do right now is to click this link
and read about how hormones have an effect on recurring yeast
infections. That webpage will also help you determine if this is a
possible problem for you so you can correct it.
Because recurring yeast infection becomes hormone dependent in the vagina and feeds on imbalances of hormones or the sugar produced by excess estrogen, and also reduces immune function; you should test your hormone levels to determine what they are or you could just treat yourself for excess estrogen, its your choice. The most accurate test is by saliva testing. This test can be done in the comfort of your own home by mail and I recommend the test below.
The 3 or 5 Panel Female Saliva Hormone Test is the best way to test for hormone imbalances related to reoccurring yeast infections.
This test for recurring yeast infection will help you find out what hormones are too high so you can take supplements that offset these high levels of hormones that feed yeast.
Short of testing, you can see if you suffer from symptoms of estrogen dominance and go from there. If you have many of those symptoms then I would seriously consider taking the supplements below.
Dr. Shalaka Samant, PhD says...
Having elevated estrogen levels due to pregnancy, taking high-estrogen birth control pills, or using estrogen hormone therapy can increase the risk of yeast infections. Excess estrogen can promote higher levels of glycogen (a stored form of glucose) in the vagina (6). Yeast loves sugar, which is also why people with diabetes, who have trouble controlling their blood sugar levels, are often at a higher risk of getting recurring yeast infections. Estrogen also reduces the inhibitory activity of epithelial cells towards Candida facilitating colonization. Estrogen also blocks T cell development in the thymus weakening immunity which may further support recurrent yeast (7).
6. Lactobacilli Dominance and Vaginal pH: Why Is the Human Vaginal Microbiome Unique? Front. Microbiol., 08 December 2016.
7. Estrogen blocks early T cell development in the thymus. Am J Reprod Immunol. 1996 Nov;36(5):269-77.
How to Get Excess Estrogen Under Control
You should take DIM which is short for diindolylmethane. Diindolylmethane is a phytonutrient found in broccoli, cauliflower, cabbage and brussel sprouts. Studies show that DIM works indirectly by changing the way estrogen is metabolized, from the ‘bad’ pathway to the ‘good’ pathway.
DIM boosts levels of good estrogens called 2-hydroxy estrogens and reduces levels of bad estrogens, which are 16-hydroxy and 4-hydroxy estrones. Both forms of bad estrogen are carcinogens and studies show that women with elevated levels of 16-hydroxy estrone have a high rate of breast cancer.
I would also take I3C Indole-3-Carbinol, which has been found to alter estrogens damaging effects on the body and the thymus by activating genes that metabolize excess estrogen. This metabolization process lowers high estrogen levels.
I3C also has the ability to alter the way estrogen is metabolized by the body and can diminish the effects of hormonal contraceptives or estrogen replacement therapy. Researchers have noticed altered lymphocyte reactivity in women participating in these two activities; an observation that indicates altered immune response.
I3C Indole-3-Carbinol also raises immune system function by protecting the thymus from bad estrogen. Healthy immune system function is necessary for the bodies fight against excess yeast and candida.
Men can also take Dim and I3C Indole-3-Carbinol to reduce estrogen levels that rise as a man ages. This especially protects against prostate cancer and unwanted muscular atrophy and weight gain.
Low levels of progesterone can be treated with Progesterone Cream, which contains USP progesterone. This is also suggested when determined by saliva testing that your progesterone to estradiol levels are low. Progesterone does offset and control excess estrogen as well.
While treating yourself for recurring yeast infection, as you get the imbalanced hormones under control, you will be depriving yeast of its main food source in the vaginal environment, mainly glycogen produced as a result of excess estrogen.
Dr. Shalaka Samant, PhD says...
Premenopausal women naturally produce hundreds of micrograms of estrogen daily, which is enzymatically converted to specific estrogen metabolites such as 2-hydroxyestrogens (2-OHEs), 2-methoxyestrogens, 16α-hydroxyestrone (16-OHE1), and 4-hydroxyestrogens (4-OHEs). 16OHE and 4 OHEs have estrogen-like activity whereas 2-OHEs have anti-estrogen-like activity (8). In recent years, natural compounds (indoles) found in the diet, specifically cruciferous vegetables such as cauliflower and broccoli, have been shown to possess antiestrogenic activity (7). The enzyme that catalyzes 2-OHEs formation is inducible by dietary modification and supplementation with the active components of these cruciferous vegetables, indole-3-carbinol (I-3-C), or diindolylmethane (DIM) (9). Other dietary components, especially omega-3 polyunsaturated fatty acids and lignans in foods like flax seed, also exert favorable effects on estrogen metabolism.
8. Estrogen metabolism and the
diet-cancer connection: rationale for assessing the ratio of urinary
hydroxylated estrogen metabolites. Altern Med Rev. 2002 Apr;7(2):112-29.
9. 3,3′-Diindolylmethane Modulates Estrogen Metabolism in Patients with Thyroid Proliferative Disease: A Pilot Study. Thyroid. 2011 Mar; 21(3): 299–304.doi: 10.1089/thy.2010.0245
Too Much Estrogen? Support Your Thymic Gland
Excessive estrogen levels have been linked to breast cancer and reduced function of the Thymic gland. The Thymic gland helps immune system t-cells that are grown in the bone marrow mature. At a certain stage of t-cell growth in the bone marrow the t-cells migrate to the thymic gland to finish their growth. Upon maturity of the t-cells, the thymic gland releases them into the body. So excessive estrogen also reduces immune function.
You can help support the Thymic Gland by taking Thymic Protein A. Thymic Protein A is a patented biologically intact 500-amino chain protein that fits into the receptor sites on T-4 cells to turn on and program the cells for their disease-fighting functions.
Following several favorable clinical studies involving both animal (Feline AIDS and distemper) and human (chronic fatigue syndrome [CFIDS] and Epstein-Barr [EBV]) subjects, Dr. Beardsley developed a unique oral delivery system for his formulation which avoided the degradation of the thymic protein in the stomach, which was a significant problem with other over-the-counter oral thymic preparations.
The scientific data gathered from these studies resulted in the awarding of a US patent to Dr. Beardsley in 1997 for both the Thymic protein A molecule and its method of production.
In the five-and-a-half years since Thymic Protein A was introduced as an oral nutritional supplement, thousands of individuals have consumed this product. Hundreds of medical doctors are using it for a variety of immune-related illnesses with no adverse reactions from this highly purified, extremely safe, low-dose protein molecule. Thymic Protein A is produced at only one site in the world, under the personal control and supervision of Dr. Beardsley. Based on his commitment to maintaining the highest scientific standards, utmost purity is assured. It is completely safe.
What to Expect When Treating Recurring Yeast Infection
I do not know how long this will take to get rid of these recurring yeast infections for each individual. You must realize, everyone is different with different physiology, has different levels of infection and no two women will have the same levels of unbalanced hormones. You may also have other health problems that can complicate this process.
However, this will get rid of this for good once you correct the underlying problems. If I were able to make an educated guess, I would say after you have been on this protocol for two to six months, your recurring yeast infection will not return again.
You may want to consider continuing to take supplements for the hormones and Profase for recurring yeast infections as a way to prevent future yeast infections, because you may not be able to fix the hormone problems permanently.
Dr. Shalaka Samant, PhD says...
Identification and treatment of the male sexual partner’s oral and penile Candida colonization also appears to be important in tackling recurring infections (10).
10. Recurrent vaginal candidiasis. Results of a cohort study of sexual transmission and intestinal reservoir. J Reprod Med. 1992 Apr;37(4):343-7.
Medical Review by Dr. Atmika Paudel, PhD
As mentioned in the above article and this one about constant yeast infections, there are many underlying causes that lead to yeast infections every now and then and make it difficult to eradicate them. This annoys a lot of people, especially women, who get vaginal candiasis. Well, if any of you are suffering from the symptoms mentioned in the above article, then you might want to check several factors that is causing your recurrent yeast infection.
First you should be able to tell that what you are getting is a yeast infection and if it is occurring quite frequently, then you should check each factor mentioned above in the article to know exactly what is causing the recurrent infections in your particular case. Sometimes, more than one factor might be the culprit. Apart from these, you might also want to know your comorbidities, if any, such as diabetes, atopic dermatitis, and use of other medications such as antibiotics and steroids, which put you at a higher vulnerability.
While I have also given similar comments in the other article, I would like to emphasize here that use of prebiotics and probiotics will help in replenishing the good microbiome of our body that might take away the recurrent yeast infections in half of the cases. Maintaining a balanced microbiome is not only good for keeping recurrent infections at the bay, but there are numerous other advantages which are beyond the scope of this comment here. The hormonal imbalance such as estrogen dominance is largely responsible for recurrent vaginal yeast infection and has been presented in detail on this page.
To summarize briefly, you should closely watch your symptoms, perform the necessary tests to confirm your suspicions, and then take appropriate actions/medications accordingly. You are the only person who knows your body the best, so work closely to find the best fit for your body and do not hesitate to seek help when necessary.
Have Any Questions Recurring Yeast Infections?
Do you have any questions about recurring yeast infections or yeast infections in general? Ask your question here or contact us using the contact page of this website. It is also always a good idea to talk to your doctor as well.
Recurring Yeast Infection Testimonials
Dan~
I felt better today after taking the products than I have in years!!!! I had more energy than ever! Is that normal to feel that different the first day? I mean I felt awful before I went to bed last night and even when I woke up this morning I still felt icky. Literally an hour after taking the Profase and Biofase I felt different. WOW! I hope that continues!
Thanks~ Emily
*****
Hi Dan,
I have suffered from recurrent yeast Infections for years and I finally
came across your product profase and biofase which have helped me
immensely! I can't remember the last time I was yeast infection free for
almost 5 months now and especially while pregnant! Your products
are amazing!
Thanks!
Megan
Recurring Yeast Infection & Women's Yeast Infection Page
Home Privacy Policy Copyright Policy Disclosure Policy Doctors Store
Copyright © 2003 - 2025. All Rights Reserved under USC Title 17. Do not copy
content from the pages of this website without our expressed written consent.
To do so is Plagiarism, Not Fair Use, is Illegal, and a violation of the
The Digital Millennium Copyright Act of 1998.